Goals of Cleft Care
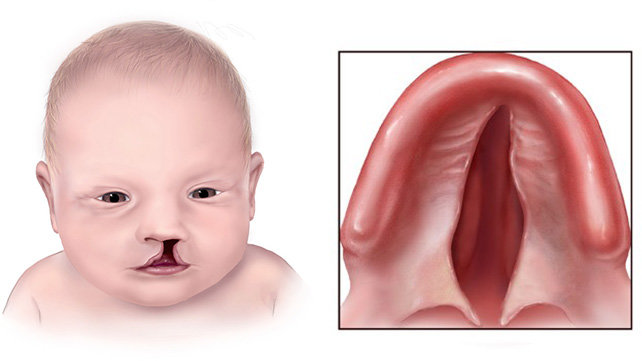
The craniofacial team’s goal is to provide your child with an attractive appearance, healthy teeth, good hearing, understandable speech and language, along with a smooth transition from home to school and other community settings. (Photo courtesy of the Centers for Disease Control and Prevention)