An Emphasis on Mutual Trust
"We are committed to making sure that before surgery, we have a mutual trust established between patient, parents and my team and they need to feel 100 percent comfortable once we make that decision.” - Ziya Gokaslan, MD

Ziya Gokaslan, MD, neurosurgeon-in-chief at Rhode Island and The Miriam hospitals, stood before his patient, a 24-year-old woman. She arrived at the Rhode Island Hospital emergency department the previous night, trembling with excruciating pain, a loss of balance and migraine.
At this moment, she was calm and comfortable, enveloped in a Halo vest, an external brace that prevents the neck and spine from moving. She looked familiar to the internationally known surgeon.
When her parents joined them, Dr. Gokaslan recognized the distraught father. He was Richard Allaire, chef and owner of a popular local restaurant he patronized, whose daughter, Isabel, he remembered seeing there. Now they were discussing the high-risk, life-saving surgery he was confident could eliminate the chronic pain she tolerated for nearly eight years.
Her ordeal had begun after an incident during a high school volleyball game that caused pain and numbness and led Isabel to seek medical attention immediately. X-ray results indicated she had a moderate case of thoracic scoliosis. Nobody realized the diagnosis was masking, and possibly worsening, a more serious condition that would come to light years later in the emergency room.
"We are committed to making sure that before surgery, we have a mutual trust established between patient, parents and my team and they need to feel 100 percent comfortable once we make that decision.” - Ziya Gokaslan, MD
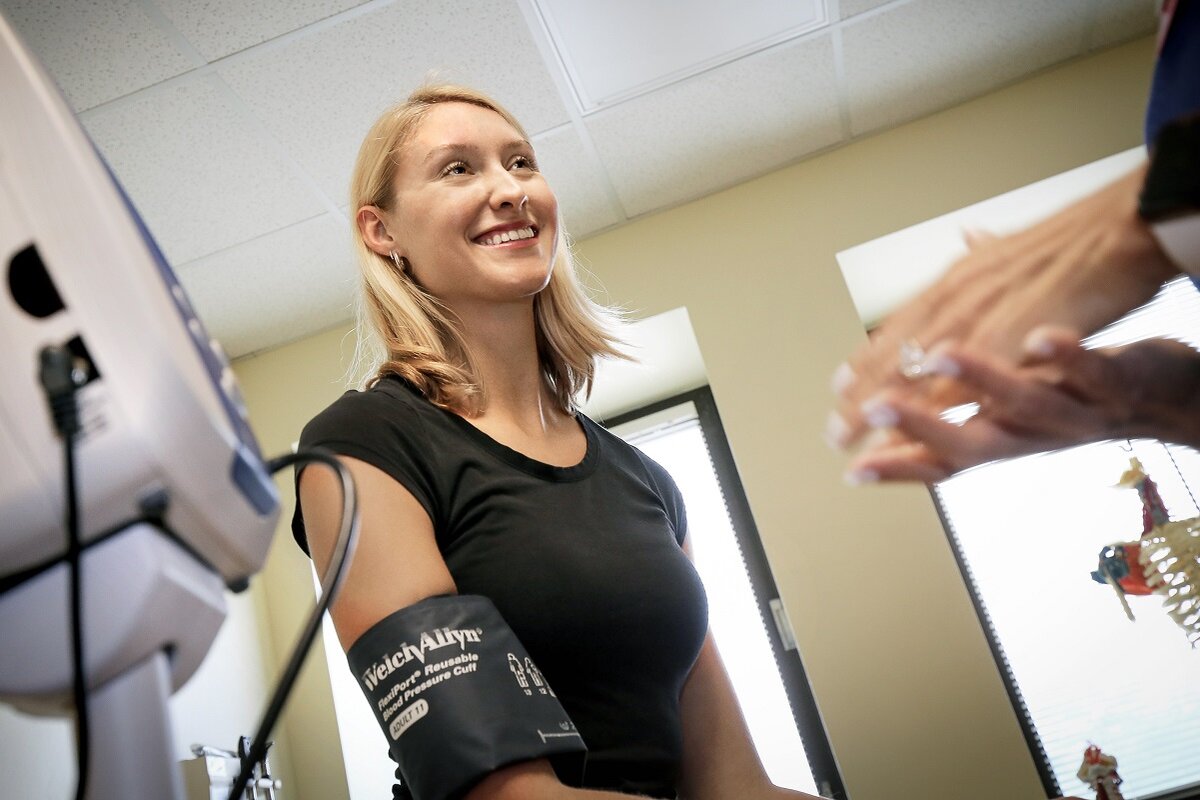
Following high school, the Rhode Island native went to the Fashion Institute of Technology in New York City and then the New York Film Academy to study film. After graduating, she launched a career in video production and shortly after started to freelance in photography and social media marketing. At six-feet tall, with shoulder-length, blond hair and a smile to light up the universe, her future was bright. She powered through the chronic pain, supplementing it with healthy living, visits to the chiropractor, scoliosis screenings, and pain-relieving massages.
“Every year, it (the pain) was getting worse,” she remembers. “My back would hurt, I felt numbness, tingles.” It finally broke her. She returned to Rhode Island for the support of her family while she reimagined her career and tried to manage an escalating health situation.
Isabel and her family had a trip to Spain planned. Leading up to their departure, Isabel was experiencing severe pain, which prompted her to go for an x-ray. The results indicated something needed further exploration and an MRI was recommended. But she was advised that it was not severe enough to cancel her trip that was in the next few days. Unfortunately, her pain followed her to Spain, and between paella and historical sites, she struggled with dizzy spells and was forced to lie still every few hours.
As soon as she returned home, she scheduled the MRI. When doctors could not detect the cause of her pain and other symptoms, they recommended she make an appointment with Brown University Health Neurosurgery, which is led by Dr. Gokaslan.
A week before her scheduled appointment, her condition intensified with migraines, dizziness, fainting, numbness on the left side of her body, and shaking. She could not wait for the appointment in few days. She called her primary doctor who sent her to the emergency department at Rhode Island Hospital.
Once there, doctors recognized a compression of her brain stem. Felicia Sun, MD, a neurosurgery resident in her fifth year, promptly ordered additional imaging. The results were extremely complex.
In addition to scoliosis, Isabel had three serious conditions: 1.) Basilar invagination, a rare condition when the top of the spine gets pushed into the base of the skull; 2.) Chiari malformation, a condition in which brain tissue extends into the spinal canal; and 3.) Syringomyelia, fluid-filled cysts or syrinx within the spinal cord. All of these added up to life-threatening pressure on the brain stem that was preventing cerebrospinal fluid, essential to the central nervous system, from flowing freely.
Despite the complicated diagnosis, Isabel was optimistic. The doctors explained that surgery would align her body and reconfigure her skull and spine, permanently. “I was excited that something was getting done and they diagnosed the problem,” she remembers. “I was hoping that it was fixable. Everyone was so confident.” She slept in the Halo, an intimidating-looking device that provides temporary comfort for patients with spinal deformities and injuries. “I had the best nine-hours of sleep of my life,” she recalls of that overnight in the emergency department.
The next morning, Dr. Gokaslan met with Isabel and her parents to explain the procedure and answer their questions. They trusted him 100 percent.
“To prepare the patient and parents for this very complicated, high-risk procedure, I assure them as best as I can that I'll do the best I can,” Dr. Gokaslan says. “I tell them, we will have the best technology in the operating room, we’re going to monitor every function, and we will be as diligent and as careful as one can be. We are committed to making sure that before surgery, we have a mutual trust established between patient, parents and my team and they need to feel 100 percent comfortable once we make that decision.”
See photos of Isabel in the halo pre-surgery and at her follow-up appointment with Ziya Gokaslan, MD.




Dr. Gokaslan and his team had prepared for the surgery, creating three-dimensional models of Isabel’s spine, reviewing specifics of the surgery, and developing alternate techniques if a procedure was to fail. The 5-6 hours of delicate surgery went according to plan. Isabel remained in the Halo vest as Dr. Gokaslan inserted, precisely, metal plates and screws into her skull, removed the base of the skull, performed a laminectomy procedure to remove the bone in the upper part of the cervical spine, and then inserted a bovine pericardium patch (expansile duroplasty). This added nearly half-an-inch to her already statuesque height. Now at six-feet and half-an-inch tall, she laughs at the thought that she was, essentially, stretched.
Within hours after surgery, Isabel was able to walk about the floor where she was recovering. Four days later, she went home for a few months-long recovery. Six months after surgery, at her follow-up appointment with Dr. Gokaslan, she told him, “I feel better than I have in 10 years. It’s like nothing happened.”
Until she needed it, Isabel acknowledged that she never realized the high-level of care that was available right in her home state. “I can’t believe I didn’t have to be airlifted out of state. People are flying (to Rhode Island) from other countries to come here for these great facilities.”
Dr. Gokaslan, who came to Rhode Island following a decades-long career with some of the country’s top hospitals, seconds Isabel’s opinion. “The quality of the healthcare we provide here is second to none. We feel very privileged that she really trusted us, and we were able to take care of her.”
Isabel now resides in her own apartment and manages her own freelance social media business. Reflecting on her medical experience, she says, “I’m feeling so lucky because right here, in the smallest state, Dr. Gokaslan was the one who could do it.”