Contact Interventional Cardiology
For more information or to refer a patient, please call 401-606-1004 or visit brownhealth.org/cardiac.

Transcatheter aortic valve replacement (TAVR) offers a lifesaving option to patients who have severe aortic valve stenosis, but who are not candidates for open heart surgery due to advanced age or existing medical conditions.
For more information or to refer a patient, please call 401-606-1004 or visit brownhealth.org/cardiac.
The Brown University Health Cardiovascular Institute of Rhode Island, The Miriam and Newport hospitals was the first program in Rhode Island and among the first in New England to provide this less invasive alternative to open heart surgery. Since December 2014, the Brown University Health Cardiovascular Institute has performed more than 1,600 TAVR procedures.
Our TAVR program is helping patients live longer with an improved quality of life.
Aortic stenosis is a progressive disease that affects approximately 1.5 million people in the United States. Approximately 500,000 of these patients suffer from severe aortic stenosis, which can restrict normal daily activities, such as walking short distances or climbing stairs, and can cause sudden death.
Aortic valve stenosis—the hardening and narrowing of the aortic valve inside the heart—forces the heart to work harder to pump blood through the body. Ultimately, the condition can weaken the heart and lead to congestive heart failure and death.
Brown University Health Cardiovascular Institute physicians use the procedure to replace narrowed and diseased aortic heart valves with artificial valves. The new valve is fed into the aorta using a catheter inserted through a small incision into a blood vessel in either the thigh or chest. Patients who undergo the TAVR procedure will, on average, spend less than a week in the hospital and should make a full recovery within two to four weeks. Our TAVR procedures are precisely orchestrated by a world-renowned, multidisciplinary TAVR team led by interventional cardiologists and cardiovascular surgeons.
Left atrial appendage closure is a procedure to protect against strokes in patients who have atrial fibrillation that is not related to heart valve disease.
Patients with Afib often take blood thinners such as warfarin to prevent clots, but a new implantable device called WATCHMAN may be a better alternative for some.
WATCHMAN is a state-of-the-art permanent implant that is used to reduce the risk of stroke by closing the left atrial appendage, where clots may form. WATCHMAN, which is implanted using a catheter-based procedure, was approved by the FDA in 2015.
The Valve and Structural Heart Program team began implanting the device in 2017, and since then has performed more than 500 WATCHMAN procedures.
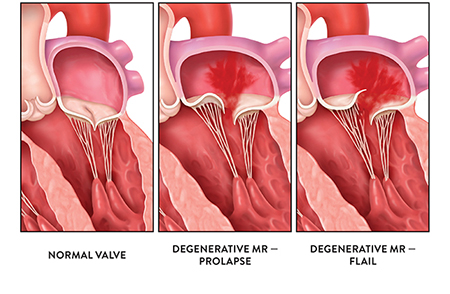
A number of mitral valve repair procedures are carried out using a catheter that is threaded through an artery to the heart. In one of these procedures, a clip is used to reshape the mitral valve and improve the flow of blood through the valve. Known as MitraClip, this treatment was approved by the Federal Drug Administration in 2016.
Since then, the Valve and Structural Heart Program has performed more than 160 of these procedures.
MitraClip is an option for patients who have severe, symptomatic, degenerative mitral valve regurgitation, but who are at too high a risk to undergo surgery to repair or replace the valve.
Learn more about interventional cardiology at the Brown University Health Cardiovascular Institute