Predicting Thumb Carpometacarpal Osteoarthritis
Are Women More at Risk?
Thumb carpometacarpal (CMC) osteoarthritis (OA) is a widespread, disabling disease of undetermined etiology that is far more prevalent in woman than in men.
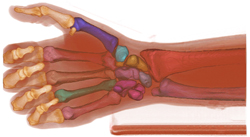
The disease affects 15% of adults over age 30, and two-thirds of women over the age of 55. Loss of thumb function alone imparts a 40%-50% impairment to the upper extremity due to its central role in nearly all grasp and handling tasks. Although recent studies suggest genetics, increased BMI and environmental factors (such as hand use) are likely associated with the development of thumb CMC OA, there is strong empirical and experimental data indicating that altered biomechanics plays a central role in the disease, and, importantly in its treatment.
CMC OA is far more prevalent in women than men, and women have flatter joint surfaces, smaller areas of cartilage contact, and higher contact pressures. The interpretation of this is that the CMC joints in women are less biomechanically stable than those in men, and consequently at increased risk for altered joint loading and the onset and/or progression of OA. At this point, however, there are no published studies of CMC joint biomechanics in normal or OA-affected individuals, nor are there any longitudinal studies of joint biomechanics as the disease progresses.
We hypothesize CMC joint laxity differs with age and gender, and that joint laxity will predict OA progression in symptomatic, early-stage patients, where CMC joint laxity is defined as articular kinematics that are abnormal in direction and/or magnitude.
This study is designed to generate foundational data on thumb CMC biomechanics in vivo by quantifying and comparing the differences in CMC biomechanics in older women (n = 11, age 45-75 yrs.) and younger women (n = 11, age 18-25 yrs.), and between women and men (n = 11, age 18 – 25 yrs; and n = 11, age 45-75 yrs.) using a cross-sectional experimental design (Aim 1), and, using a longitudinal experimental design, to determine if CMC joint laxity is positively associated with CMC OA progression 1.5 and 3 years after initial diagnosis in patients (N = 80; 45-75 yrs.) who initially present with CMC pain and minimal radiographic evidence of OA (Eaton I/II) (Aim 2).
Aim 1 will provide the first in vivo data to date on 3-D biomechanics of the CMC joint during functional tasks, which should provide insight into the role of biomechanics in the disease, and reasons for the high prevalence of OA in women as compared to men.
Aim 2 will provide the first quantitative assessment of the biomechanical changes that occur in the CMC joint during early OA progression in this population and will provide the foundation for future studies designed to evaluate the mechanistic relationship between altered joint biomechanics and cartilage degradation.
Together, these studies will provide data for the rational design of surgical procedures designed to restore, reproduce, or replace the structural anatomy of the complex CMC joint, as well as baseline data for future randomized control trials and risk factor studies.
The study has been funded by the National Institute of Health.
- Orthopedic Surgeons and Specialists in Rhode Island
- Center for Orthopedic Excellence at Saint Anne's Hospital
- Orthopedics at Morton Hospital
- Cartilage Repair
- Foot and Ankle Care
- Hand and Wrist
- Hip
- Knee
- Shoulder and Elbow
- Spine Care
- Sports Medicine
- Trauma Services
- Orthopedic Oncology
- Rehabilitative Services
-
Research and Clinical Trials
- DORSAL Program
- Research Breaks Through to the Other Side of the Blood Brain Barrier
- Bridge-Enhanced ACL Repair (BEAR)
- Cerebral Palsy: Enhancing Functional Recovery
- Finding Better Ways to Heal ACL Injury
- Predicting Thumb Carpometacarpal Osteoarthritis
- Pursuing the Promise of Smart Joint Implants
- Women's Lacrosse Focus of Bioengineering Researcher
- Patient Stories
- Assess Your Joint Pain
- The Brown University Health Orthopedics Institute in the News
